Are Subluxations Real?!?
Subluxations – a term often thrown around, especially within the realm of chiropractic care, can be a source of confusion for many, particularly those living with hypermobility.
This confusion stems from the fact that subluxations carry different definitions within healthcare.
In chiropractic terminology, a subluxation is often used to describe “joint restrictions” rather than partial dislocations.
This interpretation lacks scientific backing and can lead to misconceptions among patients. Consequently, many chiropractic institutions are moving away from using this terminology due to its potential for confusion.
In contrast, a medical subluxation refers to a partial dislocation of a joint, an experience that is well-documented and supported by extensive research. When chiropractors use the term subluxation, they may unintentionally imply to their patients that their spine is partially dislocated, perpetuating misconceptions about their condition.
Furthermore, chiropractors may suggest that they possess the ability to correct these perceived partial dislocations through manual adjustments. However, it’s crucial to acknowledge that adjustments cannot physically move bones in and out of place.
For the remainder of this blog post, we will delve into the concept of medical subluxations and explore their implications among individuals with connective tissue disorders and symptomatic generalized joint hypermobility.
Subluxation Vs. Dislocation
It’s crucial to differentiate between subluxations and dislocations as proper identification and understanding of these conditions guide appropriate treatment and management strategies, preventing potential complications and ensuring optimal patient outcomes.
Subluxations:
- Medical definition: partial dislocation
- Joint surfaces still touch but are not in normal relation to each other
- May or may not be painful
- Common in hypermobile individuals, but can be extremely painful & annoying
- May or may not self-reduce
- Not always seen on imaging
- Do not always require medical attention
Dislocations:
- Medical definition: displacement of a bone from its natural position in the joint
- Joint surfaces DO NOT touch
- Can occur in any direction, resulting in complete separation of the two bones
- Very painful!
- Will not self-reduce
- Will be seen on imaging
- Always require immediate medical attention
Signs & symptoms of subluxations or joint instability may manifest in various ways, including:
- Locking, buckling, or inability to weight bear or put pressure on the affected joint.
- Sensation of heaviness or difficulty in using the affected area.
- Surrounding musculature may feel bruised or tender to the touch.
- Physical deformities, such as the presence of a sulcus sign, may be noticeable.
- Increased fatigue in the area, even with minimal use.
- Audible sensations like popping, clunking, or clicking, which may occur more frequently and be painful.
- Emotional reactions, such as apprehension about using the joint, fear of movement, feelings of guilt and frustration, and confusion regarding the symptoms and their management.
Why Do Subluxations Happen?
Several factors contribute to our anatomy, including genetic predispositions (such as having a connective tissue disorder) or experiencing trauma. These factors may make it harder for our joints to stay stable. When our joints struggle to maintain stability on their own, we may become more prone to subluxations/dislocations.
Stability depends on three things:
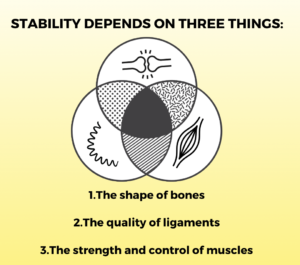
- The Shape of Bones: The shape of joint surfaces, such as shallow sockets or bony anomalies as seen in hip dysplasia, can predispose joints to slip out of position more easily.
- The Properties of Ligaments: Genetically determined variations in the structural components of connective tissue can result in ligament, tendon, and joint capsule laxity.
- Muscle Strength & Control: Altered muscle tone and impaired proprioception are common issues in the hypermobile population. Impaired joint position sense(proprioception) can lead to increased instances of bumping into objects or falling, making individuals more prone to subluxations. Certain muscles around a joint often work excessively hard to provide stability when our ligaments cannot. This can lead to muscle fatigue if unprepared, increasing the likelihood of a subluxation. Another common occurrence is performing “party tricks,” where individuals purposely sublux joints (whether for sport, performance, or to show off). This can contribute to joint instability over time, especially if done without proper preparation. Please refrain from engaging in party tricks if possible.
While the shape of our bones and the properties of our ligaments are beyond our control and typically require surgical intervention to alter, we can actively work on improving the strength and control of our muscles. By focusing on muscle-strengthening exercises and enhancing proprioceptive awareness, we can reduce the frequency and severity of subluxations, thus improving overall joint stability and function.
Is there anything we can do for them?!?
Fortunately, there are numerous effective ways to manage subluxations, reducing their frequency & intensity. An individualized approach tailored to your needs may include techniques to stabilize joints and improve muscle strength & control. To learn more about managing subluxations, book a free discovery call, and together we can create a personalized plan for YOU.
What can MSK clinicians do for their patients experiencing recurrent subluxations?
As MSK clinicians, we play a crucial role in subluxation management. From assessing severity and providing acute pain relief to empowering patients with self-management strategies, reassurance, and creating long-term strategies to decrease the intensity and frequency of subluxations. This plan may include exercises to improve joint stability, proprioception training, lifestyle modifications, and ongoing monitoring to optimize outcomes and enhance quality of life.
If you are an MSK clinician (PT, OT, Chiro) looking to better assist your hypermobile patients, check out our Hypermobility Mastery Program. Here, you will learn everything needed to create a treatment plan, starting from the initial visit, progressing through the diagnostic process, navigating the system, crafting a flexible rehab plan, and handling all the flares in between.
Disclaimer: This blog post is intended for informational purposes only and should not be considered medical advice. Please consult with a healthcare professional for personalized guidance and treatment options for hEDS or any other medical condition.

Your blog is a driving force of expertise, always providing fresh perspectives that engage your audience. It would be amazing to see you unpack how these ideas apply to modern challenges, like AI or sustainable living. Your knack for simplifying complex topics is exceptional. Thanks for sharing such transformative content. I’m excited for more!
Domain: https://gpt4geeks.com/how-to-make-chat-gpt-work-faster/
бесплатная версия ChatGPT
Your comment is awaiting moderation.